Whether they admit it or not, most healthcare organizations use temporary labor from time to time. When doing so, a typical healthcare organization reaches out to a preferred group of vendors and thus begins a process which starts with communicating the need and culminates with a check being cut by the healthcare provider sometime after the temp actually shows up and works. There are many steps in the process between those events, each with their own unique frustrations.
However, when I talk to people involved in temp staffing from both the providers and the agency perspective, there is one frustration that rises above all others. Yes, the almighty of administrative headaches for those involved in temp staffing is the invoicing and payment process. In fact, if you sit down and actually map out the typical billing process with providers and vendors (I have, and you’ll see below that it’s not pretty), you find a dizzyingly complex maze of remedial tasks involving fun things like stacks of paper, chicken scratches, inter office mail, data entry and phone call after phone call.
It’s no wonder that most staffing office managers would rather eat a dirt sandwich than call out a need out to a temp agency when they are short staffed. (Hint: there’s a happy ending…just keep reading).
A deeper look reveals inefficiency at every turn
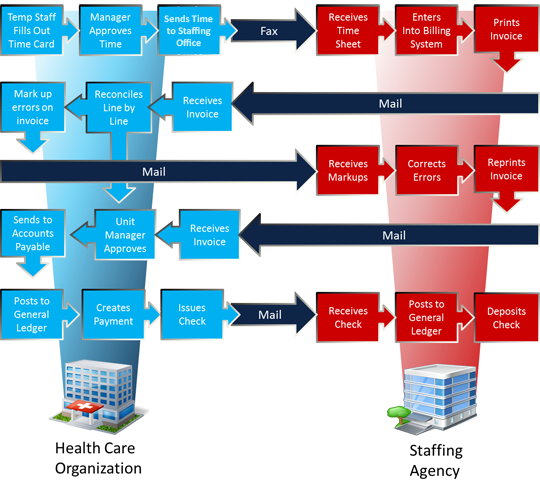
The graphic above depicts the typical “manual” agency invoicing process. To say that it is confusing, inefficient, and time consuming, would be in the top ten of historic understatements written in a blog (not sure who tracks that). To make matters worse, most health systems use more than one vendor and each comes with their own billing schedule, invoice format, coding system and abundance of phone calls trying to track down payments.
One customer I recently spoke to told me that she spends 30-40 percent of her time ensuring the accuracy of invoices she receives. And she’s just one of the many people in her organization that have to complete one of the steps in the process.
Results of our internal surveys completed by healthcare providers reveal the following outcomes of a manual process:
- The average cost (labor) to process a single invoice is $40.
- The average time spent (combined) to process a single invoice is 38 minutes.
- The average time from when a shift is worked to when the vendor receives payment is 87 days.
- The average provider pays over $1500 in postage for agency invoices per year.
- The average provider finds errors in 23% of all invoices that are submitted.
It is clear that a seemingly simple task, in reality creates a mountain of work and results in a never ending cash devouring cycle.
Automated “reverse” invoicing: A better way
If the process I’ve described sounds all too familiar; you will be happy to know that there is a better way! One of the many benefits of using a Vendor Management System (yes, like ShiftWise) is electronic time approval and “reverse” consolidated invoicing. In this model, the provider ends the use of paper timecards, eliminates the need for vendors to send paper invoices, and allows the provider to pay one invoice for all of their agency use. Furthermore, VMS applications can be customized to the unique cost centers and GL codes of the provider making reporting on costs easy and accurate. Let’s take a look at the process below to see how much easier agency payment becomes.
Results: Time, money and sanity saved
How do we quantify the benefit of a switch to VMS? According to internal surveys, on average, a provider using a VMS now spends 30 minutes of labor on the agency invoicing process per week. Cost of processing invoices goes down by an average of 87%. And job satisfaction reported by those involved in the process improves by 79%. Automating the time approval and invoicing process when using temp labor is truly one of the biggest no brainers that I can think of, and it is just one of many benefits from that can be derived by utilizing a VMS. You may still prefer to eat your dirt sandwich, dealing with agencies the hard way. But with the simplicity a VMS offers, I can’t help but wonder: why not choose the better solution?
 See demo
See demo
